For healthcare providers across North Carolina, the safe and compliant disposal of sharps—needles, syringes, scalpels, lancets, and other medical instruments capable of puncturing the skin—is a critical component of workplace safety and regulatory compliance. Improper disposal not only poses a risk to healthcare workers and patients, but also subjects medical practices to potential OSHA violations and costly penalties.
Here’s what every medical practice, dental office, veterinary clinic, and long-term care facility needs to know about proper sharps disposal.
What Qualifies as a “Sharp”?
The Occupational Safety and Health Administration (OSHA) defines a sharp as “any object that can penetrate the skin,” which includes:
- Needles
- Syringes with needles
- Scalpels
- Lancets
- Broken glass or ampules
- IV catheter stylets
- Dental wires or burs
If it can puncture the skin and has come into contact with blood or other potentially infectious materials (OPIM), it must be treated as regulated medical waste.
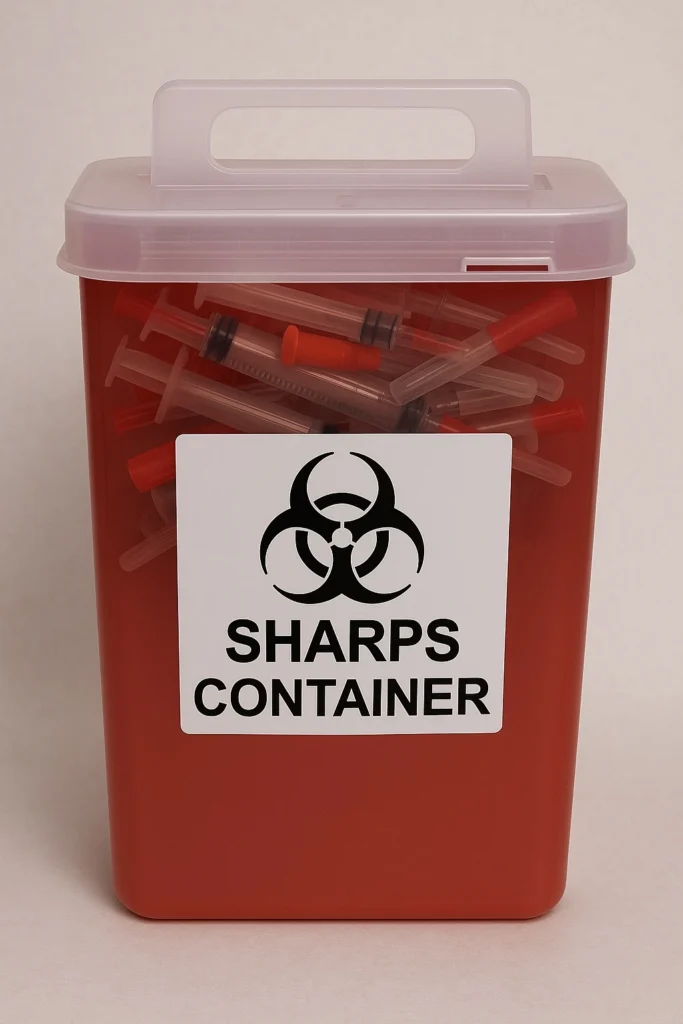
Step 1: Use the Right Container
Sharps must be disposed of immediately after use in an FDA-cleared sharps disposal container. These containers must meet the following criteria:
- Rigid and puncture-resistant
- Leak-proof on sides and bottom
- Closable and labeled with a biohazard symbol
- Easily accessible and located as close as feasible to the point of use
OSHA mandates that sharps containers be maintained upright and replaced routinely to avoid overfilling—typically when they are three-quarters full.
Step 2: Don’t Recap or Reuse
One of the leading causes of needle-stick injuries is the practice of recapping needles, which is explicitly discouraged under OSHA’s Bloodborne Pathogens Standard (29 CFR 1910.1030). Instead, all used sharps should go directly into the container without additional handling.
Step 3: Proper Packaging for Disposal
In North Carolina, once a sharps container is full and sealed, it must be packaged in compliance with U.S. Department of Transportation (DOT) regulations before transport:
- Place the sealed sharps container inside an approved outer shipping box (provided by your licensed medical waste hauler).
- Ensure the box is lined with a red biohazard bag and properly labeled with the universal biohazard symbol.
- Close and secure the box according to your hauler’s instructions. Some waste services (including BioSafe Waste) provide pre-labeled boxes with tamper-proof seals to ensure compliance and safety during transit.
Step 4: Work With a Licensed Medical Waste Hauler
Sharps should be transported and disposed of by a licensed and registered regulated medical waste hauler in accordance with North Carolina state law. Partnering with a local provider ensures compliance and improves service response. Local companies like BioSafe Waste provide:
- Regular pick-up schedules
- Emergency response for overfilled containers
- Compliance documentation for OSHA audits
Step 5: Maintain Documentation
OSHA requires that facilities maintain records of:
- Sharps injury logs (for applicable employers)
- Training in bloodborne pathogens
- Medical waste manifests from your waste hauler
These records help demonstrate compliance and are often reviewed during inspections or audits. Biosafe provides resources to clinics for training and also keep a digital record of waste manifests for all clients.
Why Proper Sharps Disposal Matters
Sharps injuries can transmit serious bloodborne infections such as hepatitis B, hepatitis C, and HIV. According to the CDC, nearly 385,000 needlestick and sharps-related injuries occur annually among hospital-based healthcare personnel in the United States. A comprehensive disposal program not only protects your staff—it’s a legal and ethical responsibility.
Biosafe Provides an Affordable and Simple Solution
Biosafe can help your business dispose of sharps waste in a compliant manner while saving your clinic money. If you are interested in our services, please fill out an interest form on our website, call us at (910) 569-9403 or email us at [email protected].